Neuropathy Treatment in Charlottesville, VA
Your body was made to heal. We help figure out what’s in the way, and what it needs to recover.
Burning, tingling, or numbness in your feet or hands shouldn’t be something you just learn to live with.
Let’s figure out what’s causing it in the first place and properly address it.
You Might Be Here Because…
If any of this sounds familiar, you’re in the right place.
What Is Peripheral Neuropathy?
Peripheral neuropathy is damage to the nerves outside the brain and spinal cord, most often in the feet or hands, that causes burning, tingling, numbness, or pain. It can make everyday life difficult, especially if it progresses. But in most cases, the damage can be slowed, stopped, and even reversed, if the root cause is properly identified and addressed.
See common symptoms and causes below.
Common Symptoms of Peripheral Neuropathy
Burning, tingling, or “buzzing” in the feet or hands
Numbness or a heavy, dead-feeling sensation
Sharp, stabbing, or electrical pain
Cramping or muscle weakness
Restless leg sensations
Balance issues or frequent falls
Cold or heat sensitivity
Feeling like socks are bunched up or walking on marbles
Nighttime symptoms that disrupt sleep
Possible Causes or Contributors
Diabetes or prediabetes (most common cause)
Chemotherapy (chemo-induced neuropathy)
Poor blood flow or circulation problems
Nerve compression (e.g., sciatica, herniated disc, carpal tunnel)
Autoimmune diseases (e.g., Hashimoto’s, Guillain-Barré)
Viral illness, including post-COVID effects
Certain medications (e.g., gabapentin, statins, Cipro)
Toxic exposure (e.g., Agent Orange, chronic alcohol use)
Vitamin deficiencies or surpluses (especially B1, B6, B12)
Surgical complications or trauma
Why It’s Worth Taking Seriously
Peripheral neuropathy isn’t just uncomfortable.
It’s a progressive condition. And if it’s not addressed properly, it often gets worse.
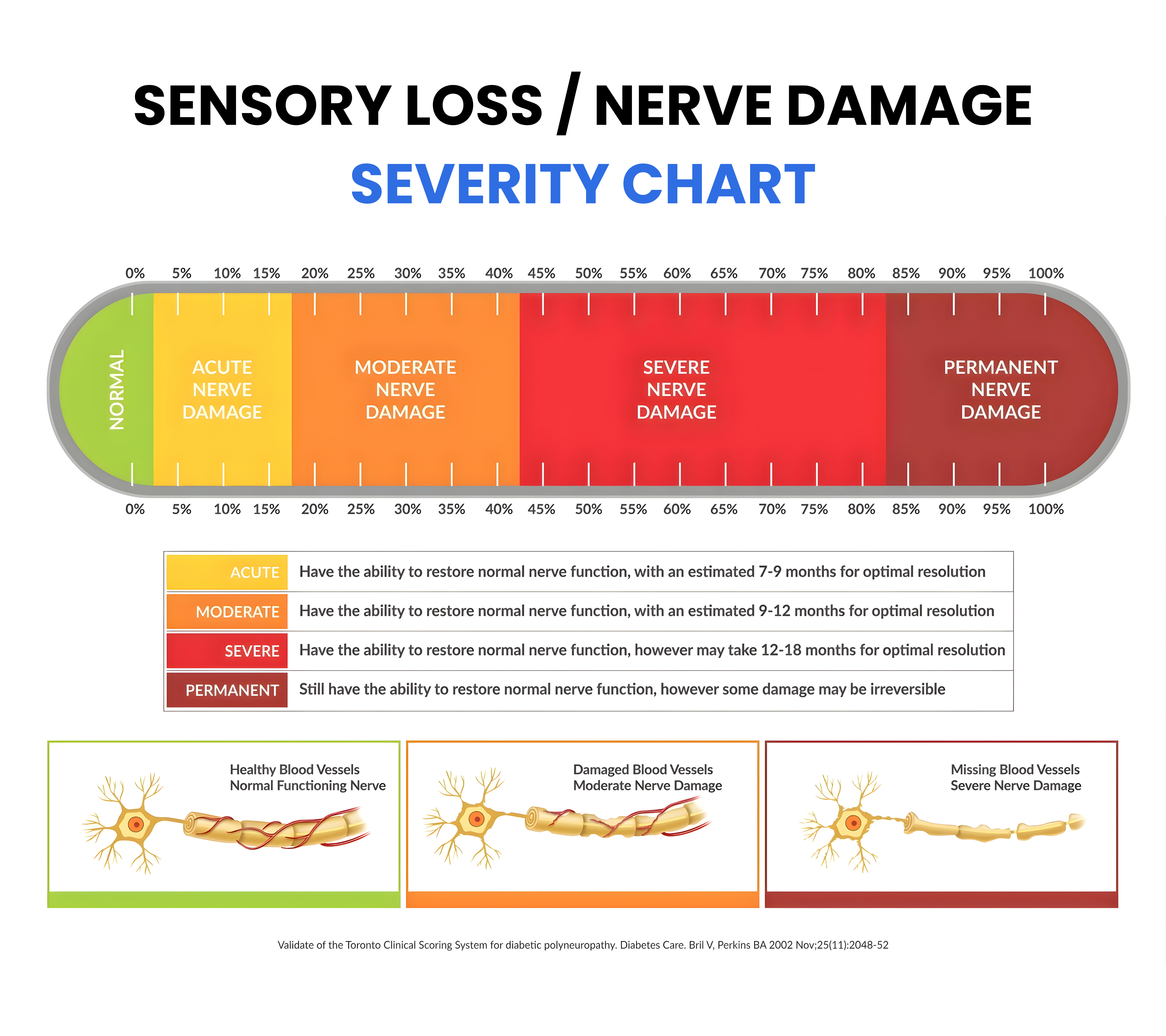
You may still be in the early stages, where nerves can fully recover.
But past a certain point, some damage becomes permanent.
We’ve seen people ignore symptoms because they “weren’t that bad yet.”
Or keep using meds that masked the pain while the damage quietly progressed underneath.
You don’t want to wait until you can’t come back.
Now is the time to find out where you stand and whether your body still has time to heal these nerves.
This chart shows what we test for during your screening and what it could mean for your ability to heal.
Why You Haven’t Gotten Better Yet
It is not because you have not tried. It is because no one has helped address the root cause yet.
Most people we meet have already spent months or years trying different solutions. They have spent money, followed advice, and done what they were told.
But the symptoms kept coming back or even got worse.
Some were told there was nothing they could do. So they settled into a life of managing symptoms, adapting to the pain, the numbness, and the imbalance. They tried to accept it, until they could not anymore.
Here is what many people have tried, and why it often fell short:
| What You Tried | Why It Often Falls Short |
|---|---|
| Prescription or Over-the-Counter Medications | Medications can reduce pain or discomfort for a while, but they do not fix the real problem. If the cause of the nerve damage is not identified and corrected, the condition can quietly keep getting worse. |
| Supplements or Diet Changes | For many, diet was part of the problem to begin with. For others, supplements or eating better helped, but nerves usually need more targeted support. There are often other factors beyond nutrition that need to be addressed too. |
| Physical Therapy and Exercise | Can improve circulation, strength, and mobility, but without knowing what is actually damaging the nerves and having a plan to fix it, progress usually stalls. |
| Specialist Visits (neurologist, podiatrist, orthopedist, etc.) | Specialists can diagnose or run tests, but most people leave without a clear long term plan. Without that strategy, the focus often stays on managing symptoms instead of helping nerves heal. |
| Massage | Can ease muscle tension, reduce stress, and improve blood flow, but it does not address the deeper causes of nerve damage. Relief is usually temporary without other support. |
| Acupuncture and Traditional Chiropractic Adjustments | These can help, especially if a pinched nerve is part of the problem, but if the compression is severe or if other factors are involved, adjustments or acupuncture alone are rarely enough to restore long term healing. |
Across all of these, the missing piece is the same: actually finding the cause of the nerve damage and creating a plan that gives your body what it needs to heal. That is what we focus on here.
How Our Approach Is Different
Most neuropathy treatments focus on managing symptoms.
We focus on helping your nerves heal.
That starts with understanding what’s causing the damage in the first place: poor circulation, inflammation, nerve compression, or something deeper. Once we know what’s behind the problem, we build a personalized plan to address it directly.
What To Expect
We keep things simple, clear, and focused on you.
1
Consultation
We start by listening. This first conversation helps us understand your full story, what you’ve tried, and what’s changed. It’s how we begin uncovering what may be contributing beneath the surface.
2
Evaluation
Next comes a series of non-invasive tests, tailored to your symptoms. These help us assess nerve function and look for key risk factors, gently and thoroughly.
Sensory Testing (Toronto Clinical Scoring System)
Different nerves are designed to sense different things — vibration, heat, light touch, or pressure. We test each one individually and compare it to a healthy area of your body.
- This helps us see if there’s loss of sensation (numbness) or hypersensitivity (overreaction).
- By scoring these results, we can identify the stage of nerve damage (there are 4 stages).
Circulation Scan (Thermographic Imaging)
Blood flow is a key factor in nerve health. Using a safe, non-invasive thermal camera, we compare temperature patterns in your feet and legs.
- A healthy scan shows even warmth.
- A diseased scan may show cooler areas, pointing to circulation issues that can worsen nerve damage.
- This test is not diagnostic, but it helps us see whether poor circulation may be part of the problem.
Reflex Testing
Reflexes help us understand how well large nerves (like the sciatic nerve) are functioning.
- If reflexes are weak or absent, it may point to a pinched nerve or another type of large-fiber dysfunction.
- This tells us whether your problem could be more structural (coming from the spine).
Spinal X-Rays (If Needed)
When reflexes or symptoms suggest a structural cause, we may take x-rays of the spine.
- We look for signs of degeneration, narrowing, or nerve impingement.
- A pinched nerve in the spine can lead to burning, tingling, numbness, or sharp electrical pain in the legs or feet.
- Seeing the spine helps us determine if the root issue is structural compression that needs to be relieved.
3
Research Phase
Behind the scenes, we review your results, medical history, and any outside records or labs. We often meet as a team to connect the dots and design a plan that fits your root cause.
4
Report of Findings
We’ll meet again, sometimes the same day or within 24 to 48 hours, to walk you through everything we’ve found. If we believe we can help, we’ll explain how. If not, we’ll tell you that too.
You’ll leave with answers, clarity, and a next step. No pressure. No surprise costs.

You’ll leave with answers, clarity, and a next step. No pressure. No surprise costs.
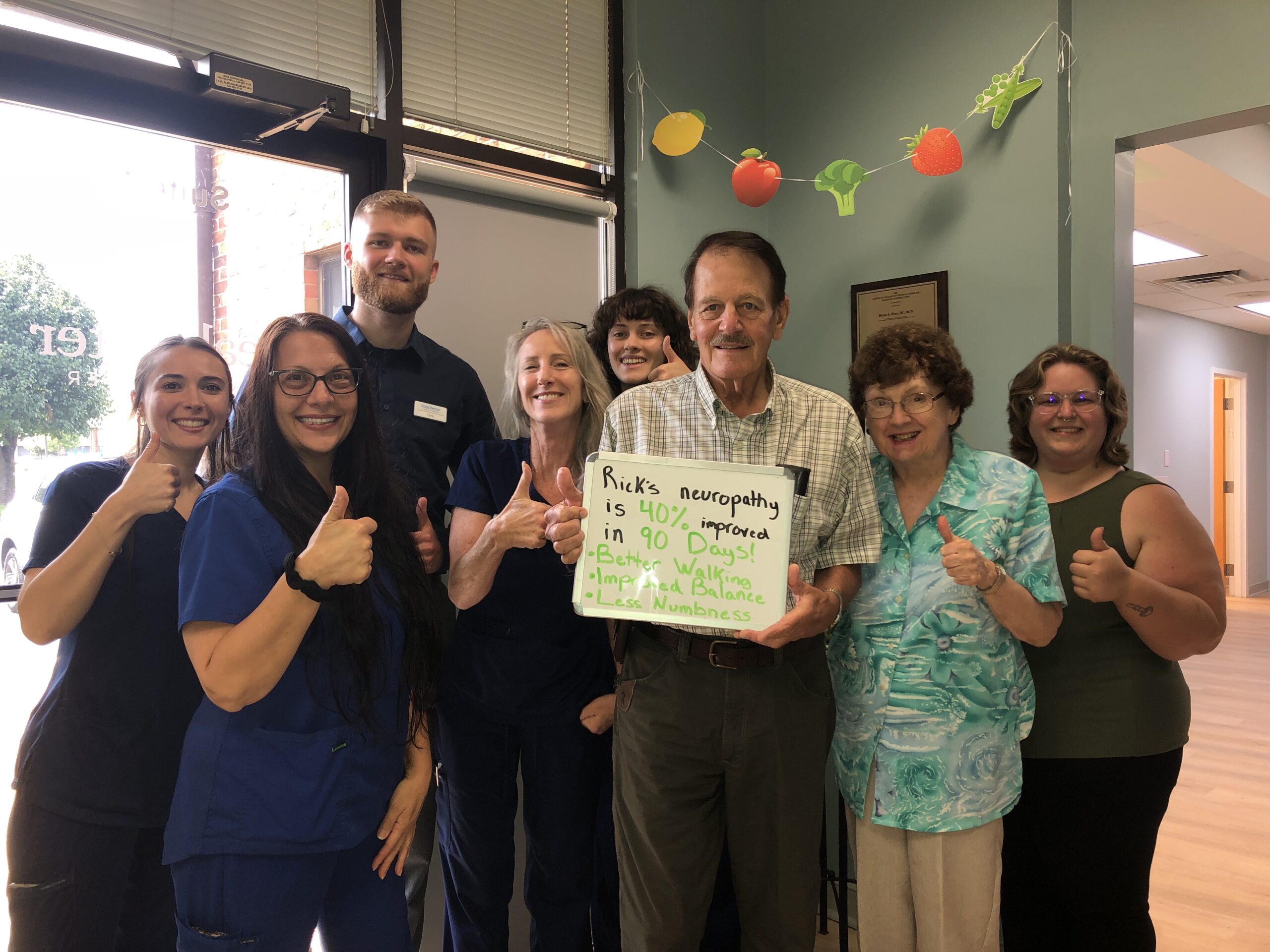
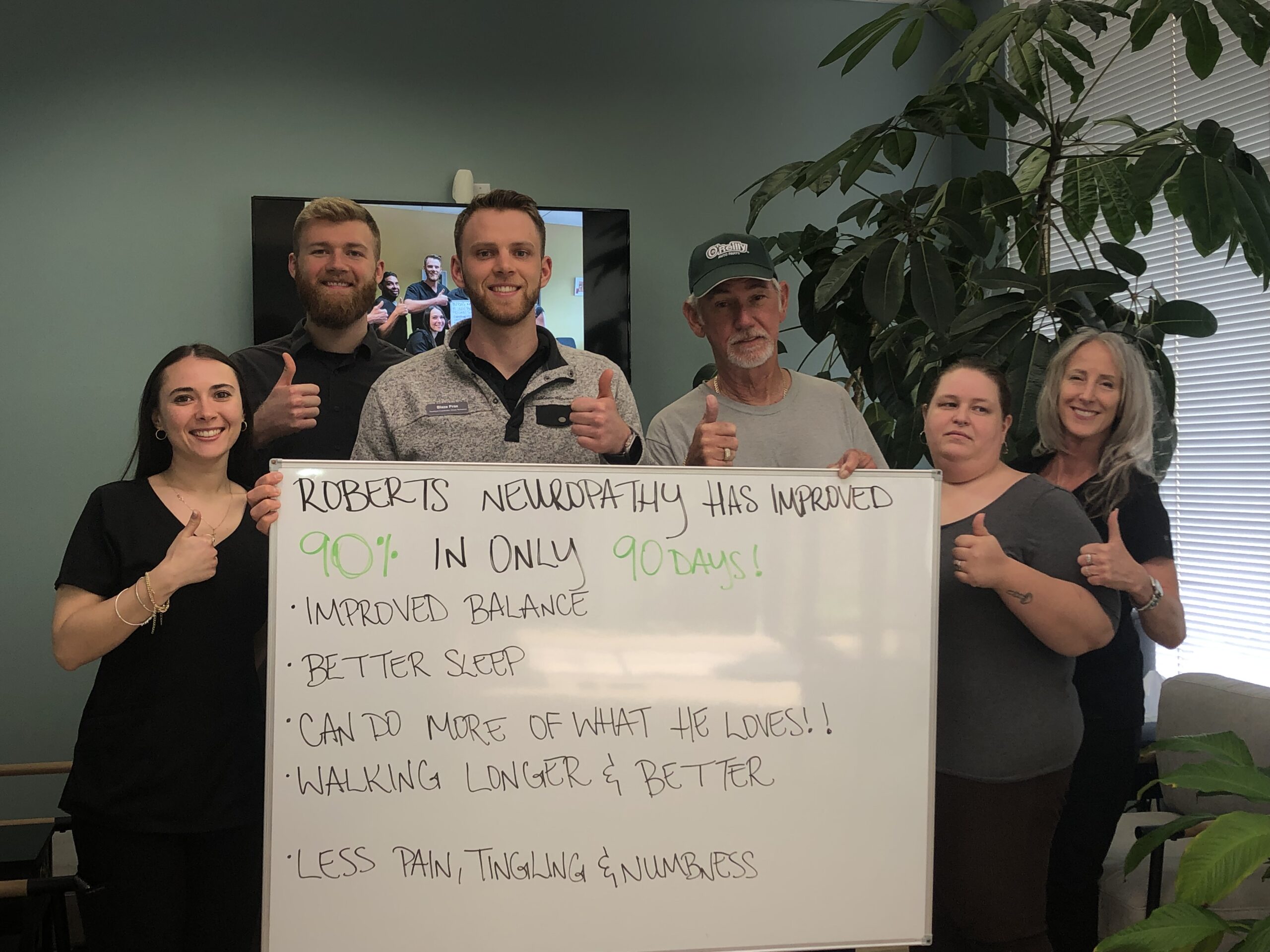
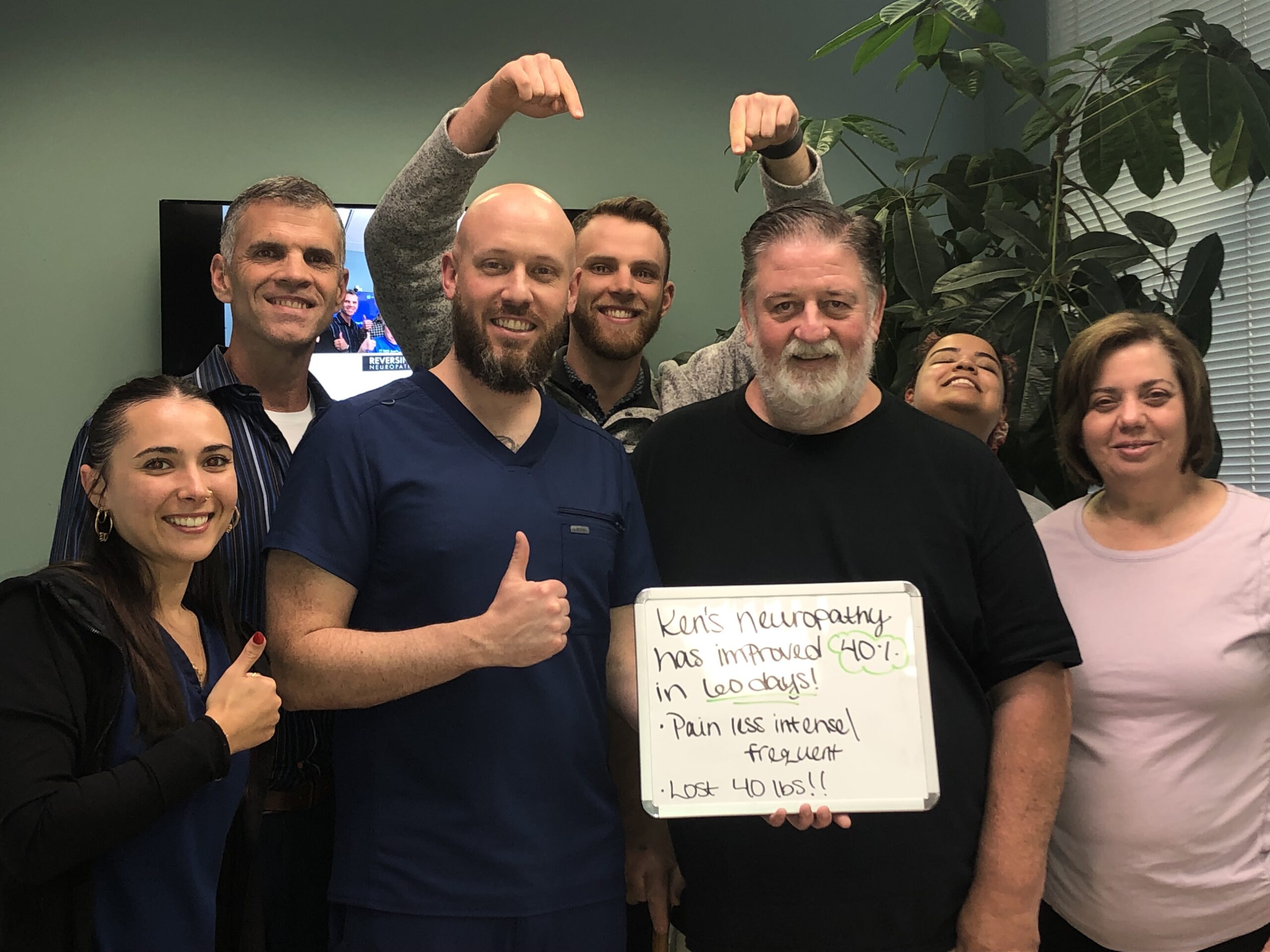
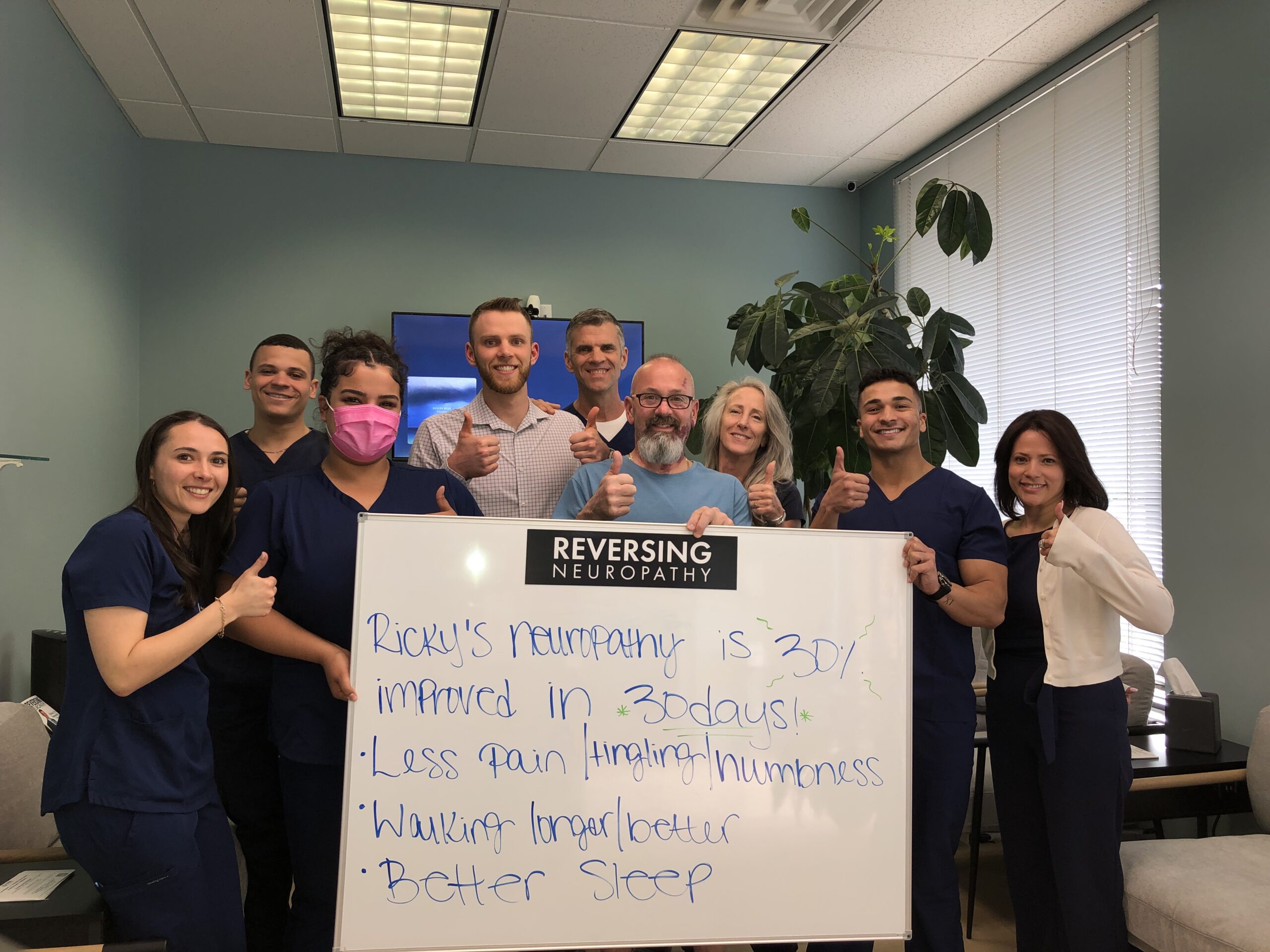
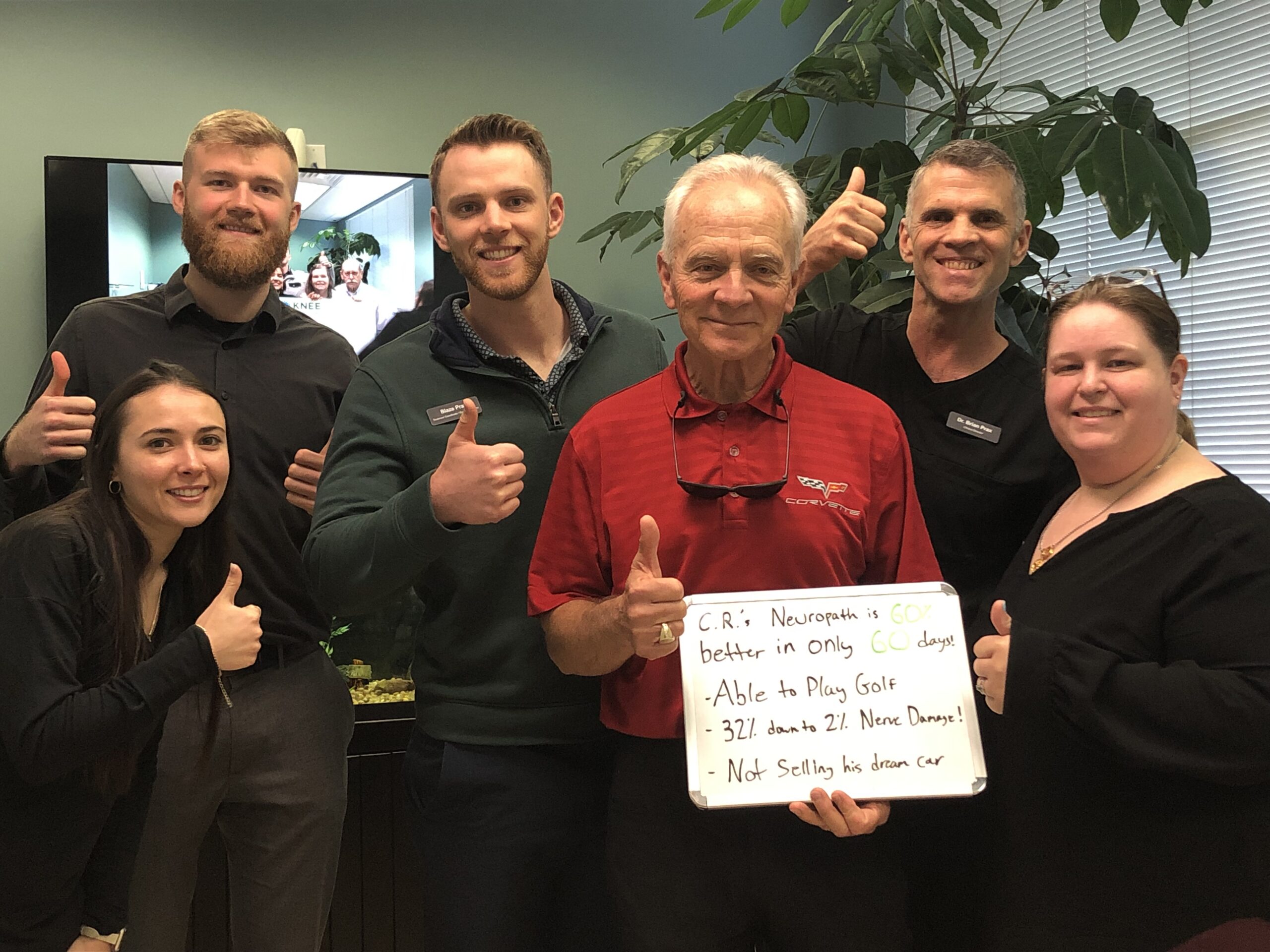
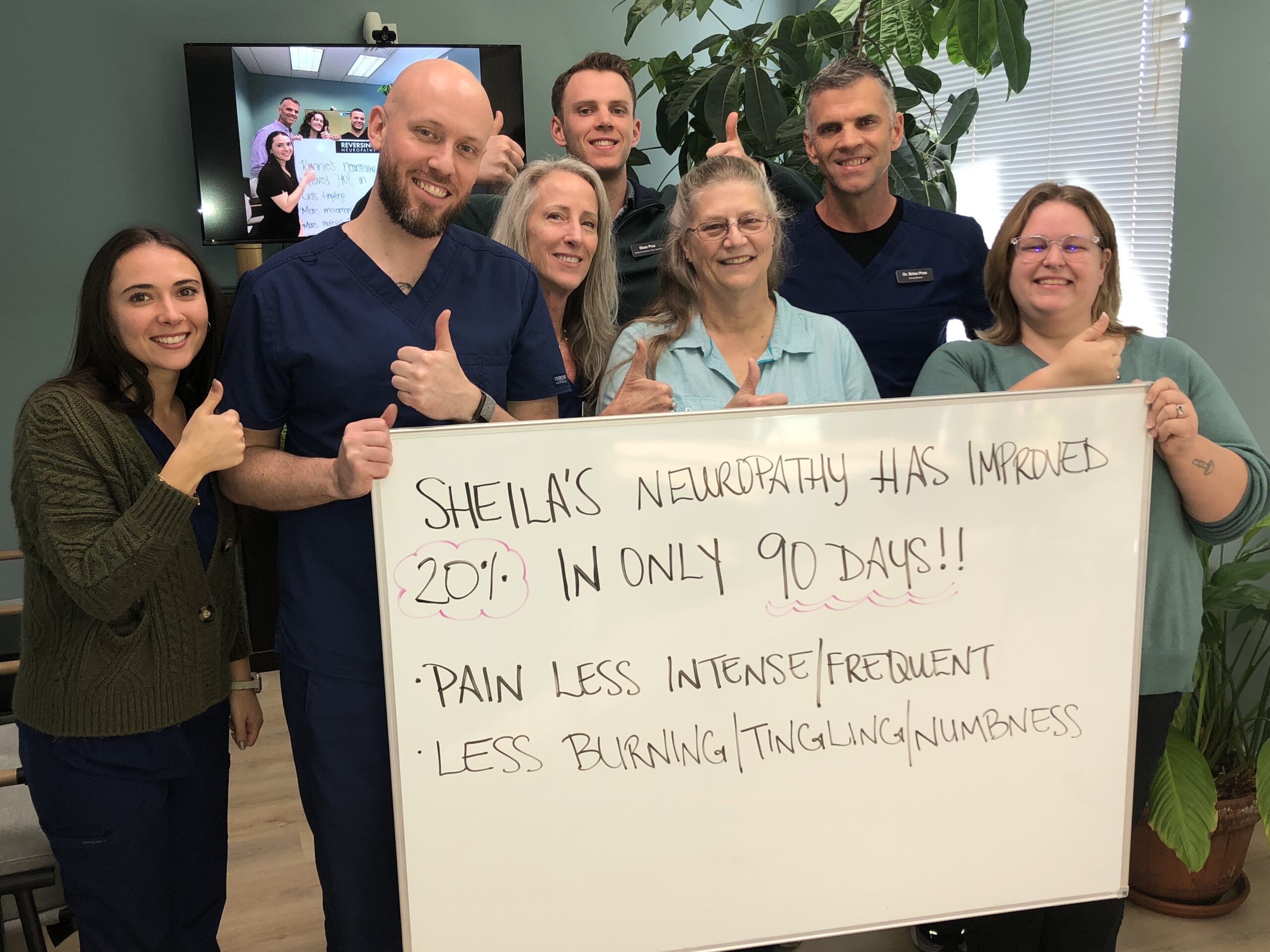
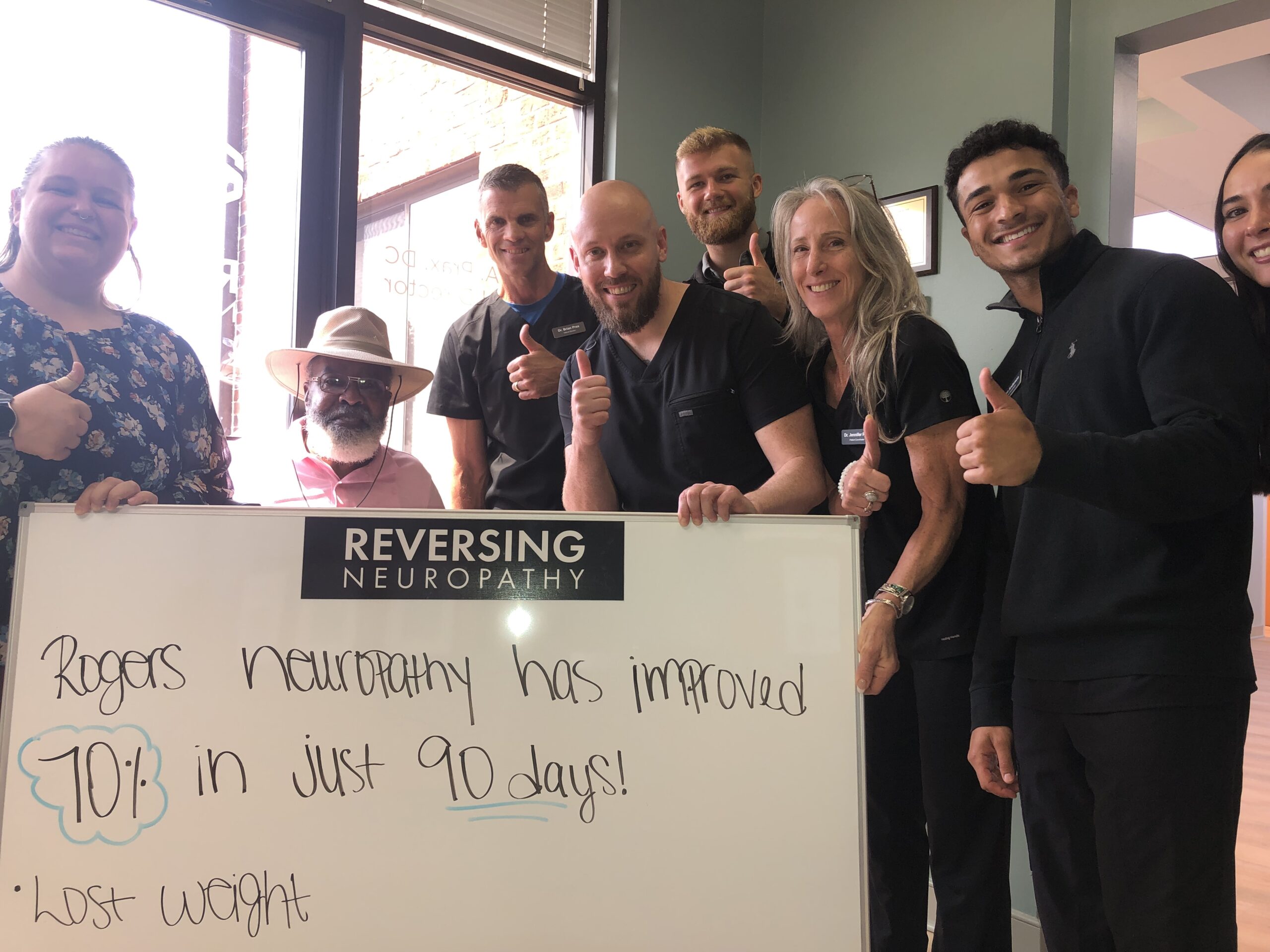
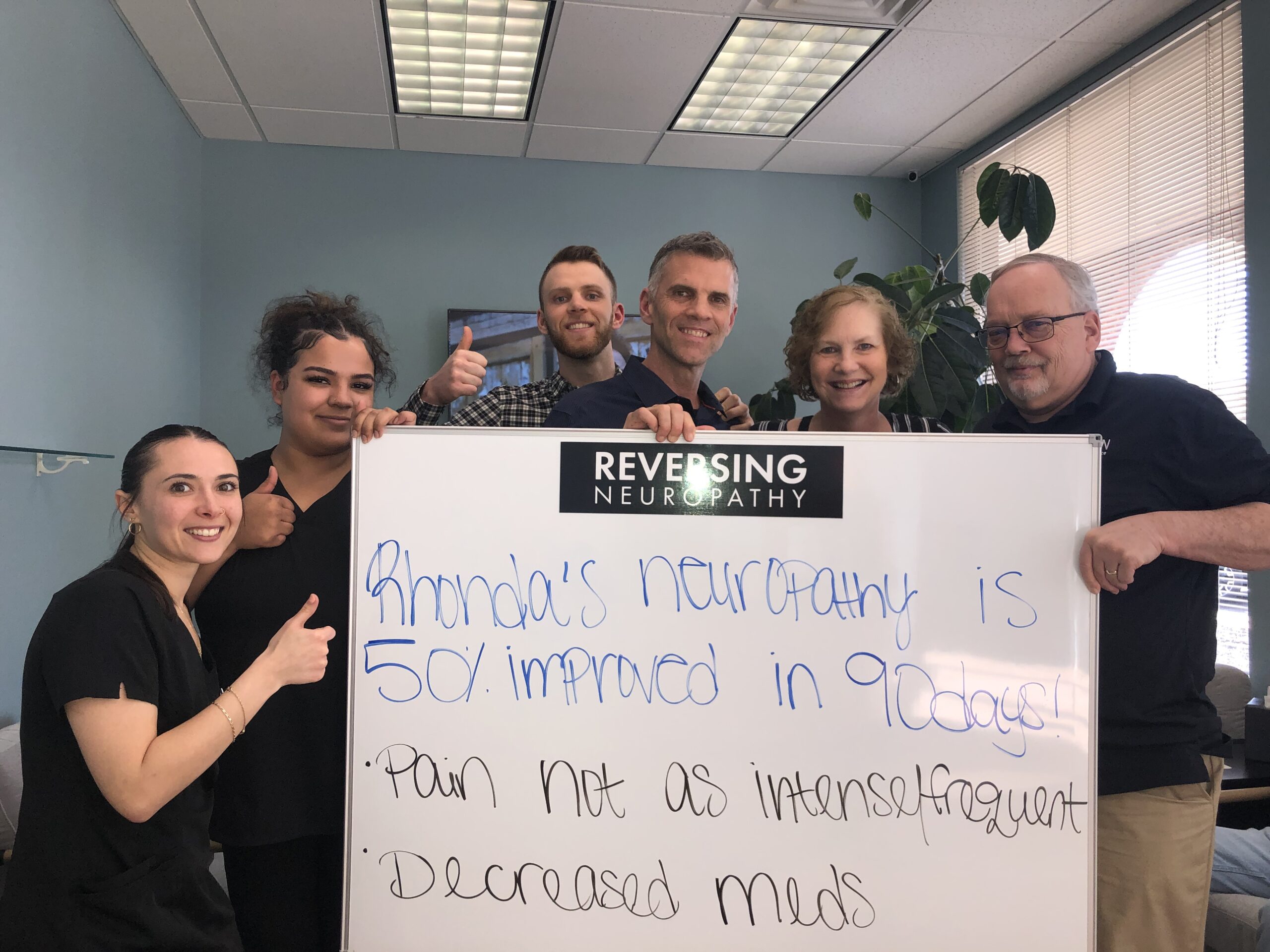
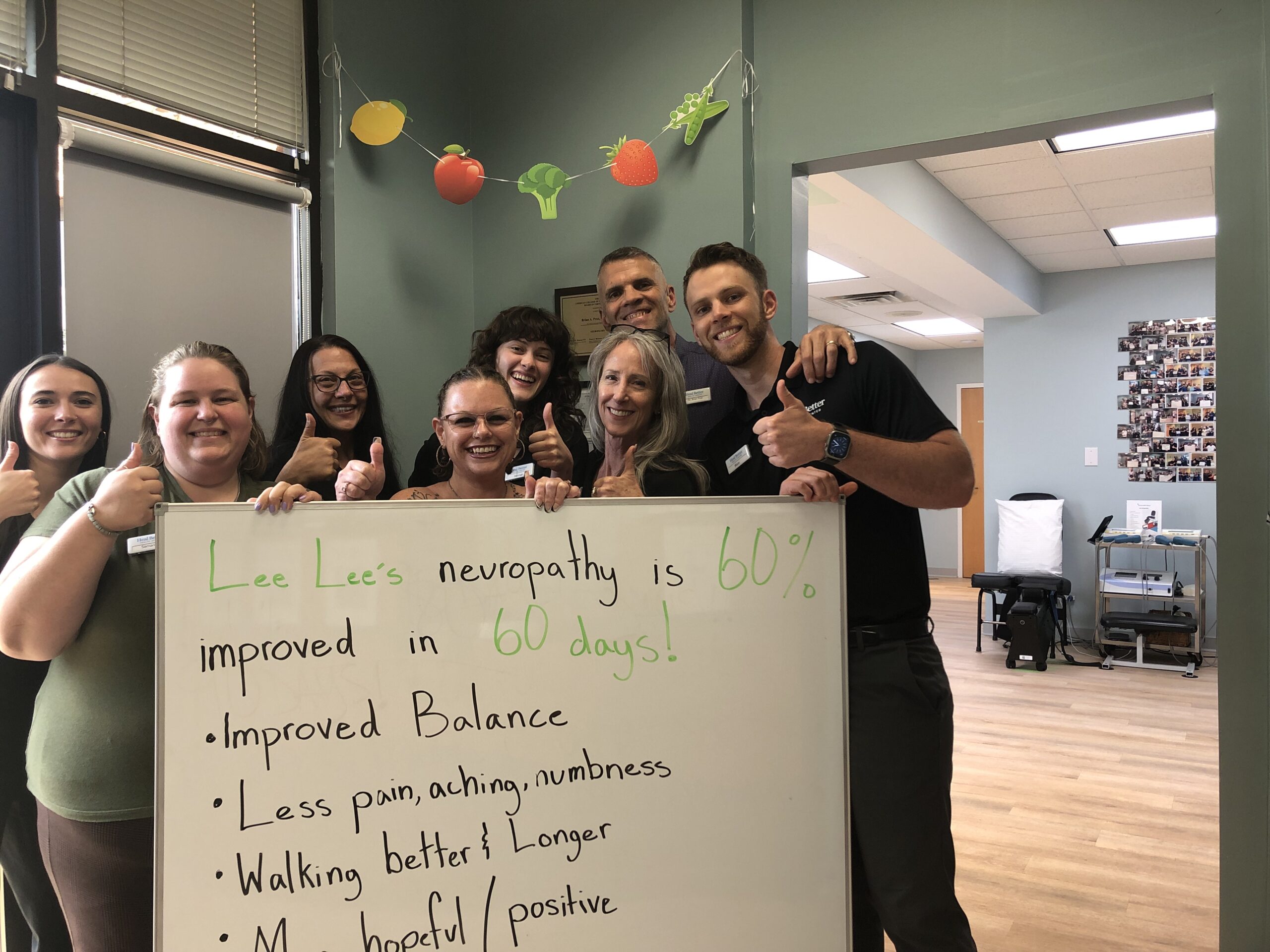
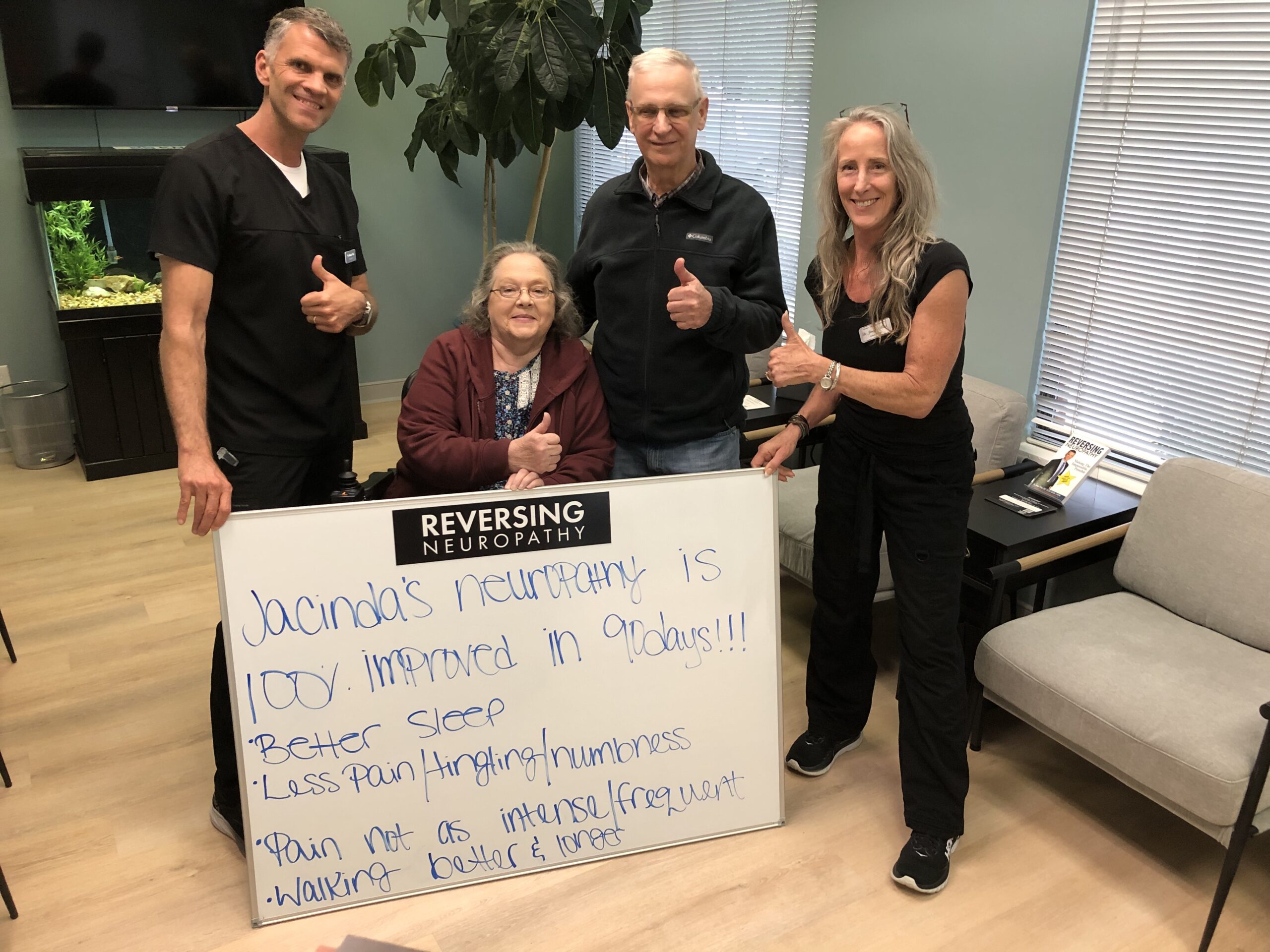
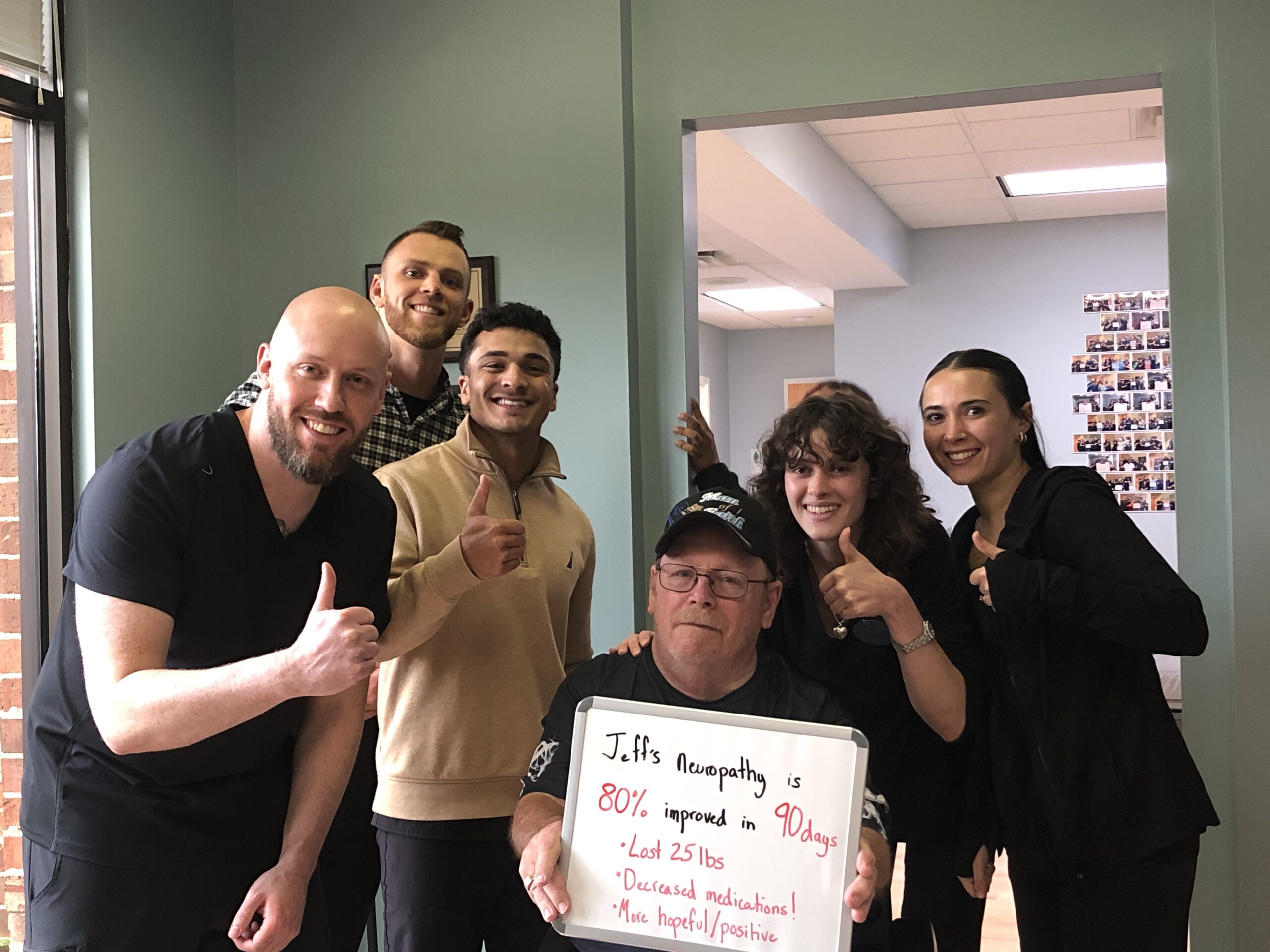
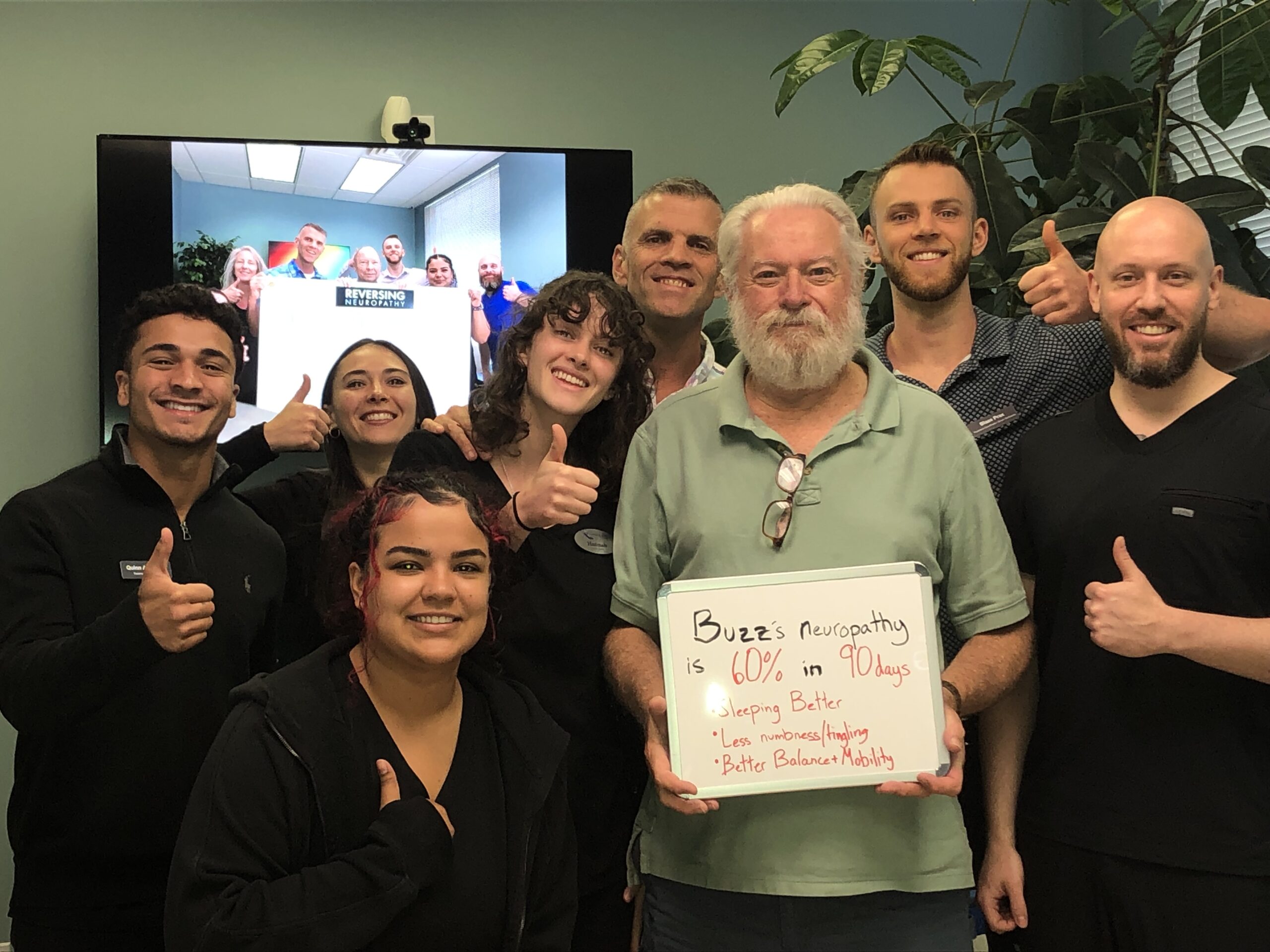
Request Your Free EvaluationHear From People Like You
No one wants to be a test case. That’s why we invite you to hear directly from real people who have walked through our doors. Some were unsure. Some were skeptical. Many were told there was nothing left to try.
Others just wanted to avoid more medication, more procedures, or a future they didn’t want to accept.
In the video below, you’ll meet a few of them. Different ages. Different stories. Different walks of life. But one thing in common: they found a path forward.
Want to hear more?
Frequently Asked Questions
Do you take insurance?
Yes. We’ll collect your insurance card at your visit. Coverage depends on your evaluation and what your treatment plan includes. Either way, you’ll know any out-of-pocket costs up front with no surprise bills.
How much does treatment cost?
Pricing is reviewed after your evaluation. You’ll know any out-of-pocket costs upfront with no surprise bills.
What treatments do you offer?
We use natural, non-invasive therapies. No drugs, injections, or surgery. Your plan depends on your condition and test results
What happens at the first visit?
You'll get a consultation, nerve testing, and a follow-up review. The entire process is free and pressure-free.
Why do I need a support person?
It helps. They may notice things you miss or understand your challenges better by being there with you.
Are you part of UVA or Sentara?
No, we're independent. But we can access your records through MyChart if needed for background.